Reimbursement Models and Their Effects on Technology Development
Satasuk Joy Bhosai, M.D., M.P.H.
Duke Clinical Research Institute and Department of Global Health, Duke University, Durham, North Carolina
Introduction
The rise of mobile and digital technologies has opened new avenues to collect and monitor important cardiovascular biometrics such as blood pressure (BP) in the home environment. Home BP monitoring not only provides an alternative to in-office measurement, but is also convenient and may be more predictive of cardiovascular events.1 Home tele-monitoring has been utilized in several BP programs and has been demonstrated to lead to larger reductions in BP and the use of less medication over time than traditional, office-based treatment plans.2,3 Based on data such as these, the American College of Cardiology, American Heart Association and European Society of Hypertension have promoted home BP monitoring as part of hypertension treatment programs.4-6 However, despite its value, the uptake of home BP monitoring remains limited in the U.S. For example, in 2009-2010, the National Health and Nutrition Examination Survey (NHANES) found that only 14-20% of U.S. individuals routinely monitored their BP at home.7
Recent advances in technology have helped overcome barriers to home BP monitoring programs. Specifically, with the expansion of cellphones, internet access, Bluetooth technology and digital health records, individuals can now easily and automatically transmit patient BP measurements to their provider. Despite these advances, the adoption of home BP monitoring has faced barriers to adoption in prior and current reimbursement environments. As this chapter will cover, the current financial and reimbursement systems have posed challenges to home versus office care and thus may impede widespread adoption of home BP programs in the U.S. In this chapter, the process of home BP monitoring, from its implementation to surveillance, is used to illustrate how reimbursement shapes the development of new technologies.
Case Topic: Home Blood-Pressure Monitoring
Prior Attempts at Storing Patient-Reported Data:
The Case of Google Health and Microsoft HealthVault Before digital BP cuffs were developed, remote monitoring systems were implemented that allowed patients to self-report their BP data into a web-based portal. Two examples of this kind of system are Google Health and Microsoft HealthVault. These systems were both originally built for a broader mission of developing a patient health record, that is, a digital home for individuals to store all their health information. Both companies used home BP monitoring as an early prototype for patient-driven data entry and home management. Google Health was launched in 2008, but by 2011, it was discontinued in part because of a failure of adoption by the provider community as well as the public.8 Some of the reasons for its failure include the following:
THE INCONVENIENCE OF DATA ENTRY FOR PATIENTS
The surgeon asked him, “What would you expect would be his prognosis in 5 to 10 years?“
LACK OF COORDINATION
Lack of coordination between data collected and actionable health interventions
For patients who did upload their data, another challenge was the lack of a formalized pathway for health providers to quickly access the information. As a result, the personal health records were poorly adopted and had limited durable users. The original leader of Google Health, Adam Botsworth, said: “My sense is that neither [Google Health nor Microsoft HealthVault] are dramatically successful. In Google’s case, it’s partly because they haven’t really pushed to see what people would want. They basically offered a place to store data. … Yes, they want to be healthy, but they need more than that.“11
LACK OF DATA-SHARING AND INTEROPERABILITY
Google Health additionally faced formidable obstacles in data-sharing between health entities. Despite partnerships with insurance agencies and hospitals, the absence of widely held standards for data-sharing between such organizations stymied interoperability between devices, the health portal, and electronic health records (EHR). Large corporate stakeholders found impediments in importing and combining information that would be readily accessible between devices and portals so that the data could be readily accessible.12,13 Furthermore, interoperability between such entities was still unwieldy. For example, if a patient had a wearable device, such as a BP cuff, it had to be compatible with his provider’s EHR provider so that the data could be imported to his medical record. Even if importing data from a third-party device was feasible, the data on the provider’s interface had to be accessible so that a meaningful review and intervention could take place.
BARRIERS TO REIMBURSEMENT
A key to making the portals both implementable and relevant to health providers is the ability of these platforms to integrate with reimbursement models. Matthew Holt, founder of The Health Care Blog and co-chair of The Health 2.0 Network, notes that it has become increasingly clear that “successful innovations that remain relevant in health systems take into consideration not only how their tools meet a need in health care, but how it saves either the hospital or insurer money.“14
The inability to provide direct means for reimbursement was also a formidable barrier in adoption of personal health records such as Google Health and Microsoft HealthVault. Remote monitoring for patients was not (and is not in a number of states to date) directly reimbursable. As former Microsoft Global Industry Director and serial health tech entrepreneur Dave Chase noted:
As much as we’d like to think it isn’t the case, the fundamental driver of most (not all) behavior in health care is the reimbursement scheme. … To understand the impact, I’ll exaggerate to make a point — your health care provider doesn’t care about you unless they can see the whites of your eyes. Why is that? Today’s flawed reimbursement scheme only compensates the health care provider for a face-to-face visit.15
Although health providers widely agree that some of their services do not require a face-to-face encounter, the ability to provide remote treatment that is directly reimbursable by health plans remains limited.
Home BP Monitoring: Considerations in Development and Implementation
Given the challenges faced by Microsoft HealthVault and Google Health with patient-generated data, these experiences can provide useful lessons for future opportunities involving patient-driven data. On a broader scale, the experience with patient-generated information can bring to light some applicable considerations to home BP monitoring. Drawing from the lessons above, the following are key considerations in the regulation of and reimbursement of remote BP monitoring:
1. Data entry must be convenient for patients. As in the case of low participation in the patient portal programs discussed above, data input must be efficient and minimize effort on the patient’s part to share data with his health team.
2. Coordination between data collected and health teams must be ensured. After data are collected by patients at home, the data should be easily accessible to health providers and provide formal means to intervene on a health condition. Moving beyond “data storing“ in third-party applications, remote monitoring devices should employ the means to communicate with health teams. Reimbursement for such communication may incentivize third parties to expand development for communication tools with providers.
3. Remote monitoring devices must be interoperable with a patient’s EHR and have data-sharing capabilities with health teams. As in the case of Google Health, despite the company’s partnerships with large insurers and hospitals, variable standards for data-sharing made the available data inaccessible to health teams. Future devices should consider the importance of interoperable capabilities so that providers and patients can act on the data. Thus, interoperability opportunities are available to encourage data-sharing between devices and health teams.
4. Cost-savings or reimbursement models must be considered. Without a means for reimbursement, useful digital technologies (such as Microsoft HealthVault or Google Health) would face ongoing challenges to scale and adoption. Digital health monitors, such as BP devices, must incorporate reimbursement models in order to scale effectively. Below, in further detail we discuss current reimbursement considerations for home BP monitoring.
Current State of Telemedicine Reimbursement
Since the early 2000s, the telemedicine reimbursement model in the U.S. has evolved. Current rules do allow for health teams to be reimbursed for time spent evaluating and managing home BP measurements. However, in its current form, this permission is not only limited to a number of states, but also often requires real-time, live interactions with providers. Telemedicine, in regard to Medicare and Medicaid reimbursement, is generally defined as, at a minimum, the use of audio and video equipment.16 This definition has presented its own challenges in the case of BP monitoring, which does not need audio or video for transmission of BP measurements. As such, in 2016, a group from the CDC conducted an environmental scan of national telemedicine programs and found that only 1 out of 53 telemedicine programs offered nationwide provided specific hypertension-management services.17
Although the federal government has made moves toward including telehealth services in their reimbursement plans, the power to determine the qualifying guidelines for reimbursement from Medicare and Medicaid largely remains with the states.18,19 Telemedicine reimbursement models vary widely by state and consequently, programs must not only satisfy federal requirements, but also meet the nuances of state-specific requirements in order for a provider to qualify for payments.20 For example, under federal standards, Medicare previously only reimbursed for synchronous, or “real-time,“ communications between a patient and provider, except for in Alaska and Hawaii. Further, it did not cover any store-and-forward services or remote patient monitoring for chronic diseases, except for the aforementioned states.21 In North Carolina, for example, reimbursement for “telemedicine“ requires “two-way, real-time interactive audio and video between places of lesser and greater medical capability.“ Furthermore, store-and-forward services, such as having BP readings stored in a portal for a provider to then review, are not currently reimbursable under Medicare and Medicaid in North Carolina and over 25 states across the country.22
States are now allowed flexibility in reimbursing for services offered via telehealth (that are not covered by federal definitions), through the submission of state plan amendments (SPAs). Consequently, the numbers of states reimbursing for store-and-forward services has been expanding. In 2016, only nine states reimbursed for such services, but now 15 do.23,24
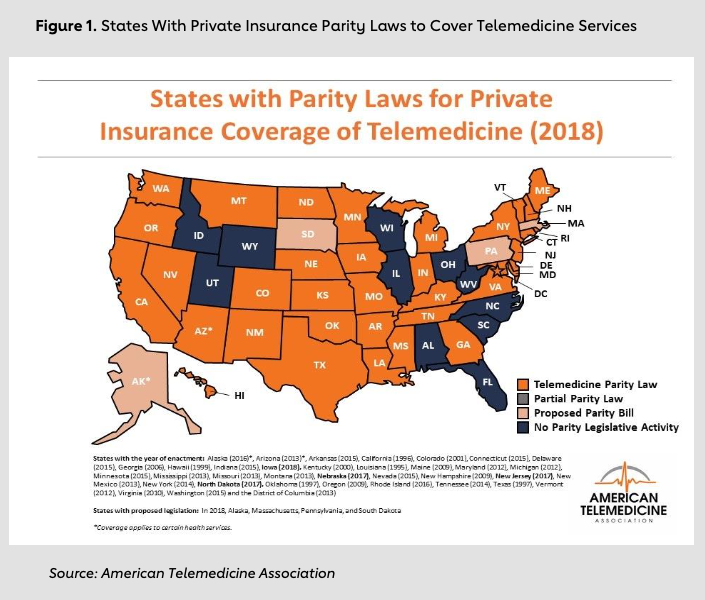
State laws have shaped some private-payer telehealth reimbursement policies. From the private-payer standpoint, several states have mandated “parity“ for reimbursement services offered between in-person health services and telehealth services.25-27 For instance, if an in- office visit for a chronic condition offers the same type of management that may be done remotely, the private payers are required to provide comparable reimbursement. Note that without parity laws, health plans can choose to pay only a percentage of what they would reimburse for in-person services. According to the American Telemedicine Association, over 30 states have either mandated private payers to provide parity in reimbursement or have proposed legislation considering parity.28,29
Additionally, private payers, such as large insurance companies like Aetna, have been known to be early adopters of telemedicine, even prior to states widely enacting parity laws. Aetna, for instance, partnered with Relay Health in 2006 to provide telemedicine offerings to its clients, citing that telemedicine “significantly reduce[s] costs by reducing non-medically necessary ER visits and readmissions as members use virtual options for after-hours care and provider instruction.“30 Since that time, they have also partnered with Teledoc, to offer expanded telemedicine services such as teledermatology and mental health services that are not required by Medicare or Medicaid in many states.31 hus, despite the lack of federal requirements, private payers have been willing to reimburse for services, recognizing that telemedicine may help with overall cost reduction in care for patients.
Current State of Remote Patient Monitoring
With the shift for bundled payments and recent government incentives to report quality outcomes, the drive to further develop home-monitoring systems has amplified recently. Since Microsoft HealthVault, multiple advances have been made in the evolution of technology for home BP measurement and monitoring. New population health companies that highlight home monitoring have emerged over the last few years. For example, Withings, a company that offers Bluetooth-enabled weight scales and BP cuffs, and Livongo, a personalized management platform for patients, offers real-time data tracking and pattern monitoring, are recent entrants in this evolving market.
Some startups have emerged that have focused exclusively on home monitoring and remote patient-provider communication. For example, WellDoc’s BlueStar product, an FDA-cleared digital coaching application that providers can prescribe to patients, has recently added hypertension to its care-management tools.32 Hale Health is a digital health tech company that connects patients and providers between appointments through secure messaging, live video and photo sharing. Its model is to help clinical teams increase capacity and improve access to care and information from health providers. Omada Health, a company focused on remote digital care management, recently added home BP monitoring to its current chronic-care offerings, providing patients with remote monitoring tools, behavioral counseling and medication-adherence features.33
Some health systems have been at the forefront of home BP monitoring. In 2013, JAMA reported promising results for a cluster-randomized control trial from HealthPartners Medical Group, showing that telemonitoring decreased home BP at six- and 12-month post-intervention follow- ups.34 Since that time, Oschner has launched its Hypertension Digital Medicine Program, which provides patients with remote digital BP cuffs and care teams to help manage their medications.35 As digital offerings continue to expand, greater opportunities have emerged for integrated management of home BP monitoring.
New Opportunities With Changes in Reimbursement
Despite limited avenues for direct reimbursement, home monitoring may currently provide cost- savings benefits for health systems, particularly where shared-savings or bundled-payment schedules are applied. Consequently, telehealth and home-monitoring initiatives have been evaluated by health systems to determine whether they can assist in bundled-payment models, where a specified amount is allotted for taking care of a condition, regardless of the number of tests, orders or evaluations that are done. For example, in September 2017, Nemours Children’s Health System found a cost savings of $24 per patient in using telemedicine to treat sports injuries.36
Additional changes may encourage further innovation for home-monitoring tools. Although these proposals have not been finalized, the following two recommendations for changes were put forth in November 2017: First, the Centers for Medicare & Medicaid Services (CMS) proposed new billing codes for virtual visits that involve care planning and risk assessments as part of CMS chronic-care management. Note that these codes are for virtual, real-time visits, which although they do not explicitly involve remote monitoring of vital signs, may suggest a growing expansion of reimbursable services.37-39 Second, Congress passed the VETS Act (H.R. 2123), which proposes an Anywhere-to-Anywhere initiative that will offer virtual consults to patients, regardless of geographical location.40,41 This recognition by the federal government of expanded telehealth services includes both synchronous and store-and-forward features, and sets a precedent for virtual care across state lines. This development may provide the basis for more flexible regulation of telehealth services across states in the future.
Avenues for reimbursement in home monitoring have begun to make way for new models for bundled payments and cost-sharing with CMS. Some pay-for-performance models are currently being revised to reflect the changing landscape of delivering care. Over the past decade, Medicare has implemented pay-for-performance measures that rewarded providers that meet a number of quality metrics, such as process metrics that improve efficiency, care coordination and health outcomes.42 However, a recent 2017 systematic review, funded through the Department of Veterans Affairs, evaluated 69 studies on pay-for-performance outcomes and concluded that improvement in health outcomes were inconsistent across pay-for- performance models.43 Consequently, in January 2018, the Medicare Payment Advisory Commission (MedPAC) recommended that Congress repeal many existing pay-for-performance programs, imposed by Congress in 2015, because the programs were found to be costly and variably effective. It called for new models to effectively incentivize health systems. 44
Some of these new models acknowledge that Medicare billing must more accurately reflect the effort and time spent on managing chronic conditions, including time spent on reviewing remote data. In January 2018, the government took steps to unbundle CPT code 99091, to allow for billing Medicare “for time spent on collection and interpretation of health data that is generated by a patient remotely, digitally stored and transmitted to the provider, at a minimum of 30 minutes of time.“45,46 Unbundling CPT 99091 allows providers to bill separately for time spent reviewing remote data. Previously, CMS did not allow remote care tasks to be billed during a service period when the patient was already being billed for chronic-care management codes such as those used for diabetes, hypertension, cardiovascular disease and chronic obstructive pulmonary disease.47
Although value-based models have been in flux over the years, BP control has remained a key indicator of quality. The National Committee for Quality Assurance, a private not-for-profit dedicated to reporting-quality metrics for health organizations, has developed HEDIS (Health care Effectiveness Data and Information Set) measures to accredit health systems for meeting high-quality care standards.
HEDIS measures evaluate the following BP metrics:
- Adults 18-59 years of age whose BP is <140/90 mm Hg.
- Adults 60-85 years of age, with a diagnosis of diabetes, whose BP is <140/90 mm Hg.
- Adults 60-85 years of age, without a diagnosis of diabetes, whose BP is <150/90 mm Hg.34
Performing well on HEDIS measures allows health systems to negotiate contracts for bundled- payment options with both private and public payers. Because over 90% of health plans use the HEDIS tool to determine performance of a health system, this development may translate into large reimbursement incentives for health providers.48
Federal Regulation as a Catalyst to Increase Digital Technology Uptake
In addition to new reimbursement models for home BP programs, other avenues exist for the federal government to incentivize broader uptake of home BP technologies. To date, the government has had to adapt quickly to the advent of new technologies. Only a little more than 10 years ago, smartphones, tablets and web-based digital health products were introduced to the public. The first iPhone was released on June 29, 2007, and not until 2011 did The White House first recognize and promote the benefits of cloud-based technologies in governmental agencies, such as Veterans Affairs and the Department of Health and Human Services.49,40 Since that time, the rise of web-based and mobile technologies in health care has dramatically changed the way in which health initiatives have harnessed the use of digital technology to accomplish project goals and study health outcomes.
The rapid growth of mobile technologies and innovations has recently led to over 3 billion unique mobile users worldwide, providing the opportunity for significant data collection and transfer between individuals, groups and organizations.51 With the rise of digital technologies, federal agencies have taken actionable steps to not only ensure adoption of digital health innovations, but also to facilitate the development of innovations.
The federal government’s role in increasing the use of electronic medical records is a prime example of how regulation can lead to digital transformation. The first attempts to spur digital health innovation were made evident through the enactment of the Meaningful Use via Health Information Technology for Economic and Clinical Health (HITECH) Act passed in 2009.52-54 The concept of Meaningful Use was founded on the idea that technology would be “meaningful“ if it met the following five goals:
- Improve quality, safety, efficiency, and reduce health disparities
- Engage patients and families in their health
- Improve care coordination
- Improve population and public health
- Ensure adequate privacy and security protection for personal health information
The Centers for Medicare & Medicaid Services provided incentive payments for health providers that demonstrated efforts to implement digital technologies that led to meaningful use. Payments were around $50,000 for private health providers but could lead to a reduction in reimbursement by up to 1-3% in Medicare/Medicaid fees if not adopted by 2017.55 As of 2016, the Office of the National Coordinator (ONC) for Health Information Technology (HIT) reported that over 95% of all eligible hospitals met meaningful-use standards through adoption of certified HIT.56
Since Meaningful Use and the HITECH Act, ongoing federal incentives and regulation to support the scale and adoption of digital health tools have proved to be strong catalysts. Shifts in reimbursement models such as those set forth by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 have fostered space for digital health technology in population health- management initiatives and quality metric reporting. With MACRA, health providers and health systems would be reimbursed in one of two ways: The first is a merit-based incentive payment system (MIPS), which weighs electronic-health-records system use and practice-improvement activities by 25%; the second method is via advanced alternative payment models (APMs), which allow health systems to get reimbursed on a fee-for-service basis but require shared payments, quality measurements and meeting performance benchmarks.57 Delivery reform efforts for these models incorporate former meaningful-use criteria, such as highlighting the need for interoperable digital health platforms and deployment of tools aimed at improving health outcomes. The reimbursement shift not only refocuses efforts on providing a service or using technology in caring for patients, but also catalyzes providers to leverage technology to improve health outcomes.
Regulation in Support of Innovation
In addition to encouraging adoption of technology in health care, the government has also made efforts to facilitate the development of new digital products. To accommodate innovation in digital health, the Food and Drug Administration announced in 2017 the launch of a Software Pre-Certification Pilot Program, which takes a pragmatic approach to evaluating health technology that breaks from its traditional model of evaluating conventional technologies, such as medical devices. The FDA has stated, “The FDA’s traditional approach to medical devices is not well-suited to these products.“58 The agency recognizes that the process for federal approval of software products must be streamlined, because digital technologies undergo multiple iterative versions at a faster pace than tangible products such as medical devices.
Digital technology and version releases often move faster than public policy and conventional approval processes. This move by the FDA demonstrates the growing recognition that applying the same regulatory rules for pharmaceutical and devices would, simply put, be an innovation roadblock for health-tech companies. The pilot program is currently underway in 2018, with its inaugural cohort to be announced later this year. The impact of this program could mean that medical software and digital health companies could curtail the rate-limiting step of federal evaluation and traditionally lengthy approval process prior to going to market. Pre-certified groups would be able to submit general information before commercialization if they are able to meet pre-qualifying FDA criteria. The fact that the FDA is engaging innovators through a more “agile“ process of approval has set a tone for rapid deployment of digital technologies for the coming years.
Opportunities and Stakeholders
Remote home monitoring has demonstrated cost savings for health providers and health systems in a few areas. For instance, home monitoring has been tied to decreased medical spending per patient, reduction in non-emergent ER visits, reduction in inpatient admissions and reduction in outpatient specialty clinic visits.59,60 The potential for digital innovations to catalyze cost savings could provide stakeholders enough incentives to adopt these technologies.
As digital technologies become increasingly widespread in health care, reimbursement changes have occurred over the past decade that aim to drive digital innovations in health care. From the HITECH Act to now the unbundling of CPT codes to allow billing for time spent on remote monitoring, health systems are incentivized to integrate digital tools into clinical practice. Providers will not only be required to meet ongoing performance measures for BP control, such as HEDIS metrics, but may also now be reimbursed separately for spending time evaluating home BP metrics.
Given that the climate for reimbursement emphasizes efficiency and quality outcomes, the coordination between providers (e.g., primary care and specialty clinic providers) might become increasingly relevant in the years to come. Further avenues may focus not only on developing pathways for groups to share methods for the data acquisition of remote BP measurements (i.e., methods to efficiently import data into a database or the cloud), but also on highlighting the need to share basic or similar data (i.e., vitals for certain time periods, etc.) among primary and specialty providers. General data-sharing policies can arguably not only improve efficiency, but also help streamline requirements needed for reporting to assist in reimbursement, evaluation of quality metrics and determination of health outcomes.
Conclusion
The move toward revised payment models has incentivized health systems to find efficient, financially viable and scalable solutions that foster high-quality care and challenge the status quo of conventional care-delivery models. Due to the dynamic and changing landscape of ongoing health reform, such as reimbursement models that shift from fee-for-service paradigms to alternative payment models, the opportunities to implement novel delivery paradigms has become increasingly clear.
Previous experiences have demonstrated that the development of technology in of itself is simply insufficient to drive widespread adoption. In the past, Microsoft and Google faced barriers to scaling, largely due to the reimbursement environment in the early 2000s. However, with the changing climate of reimbursement and progressive modifications in regulation, new opportunities in home-based blood-pressure monitoring have emerged. Given that the reimbursement environment has evolved to foster the integration of home-based digital products in clinical practice, health providers are now equipped with new tools to provide high- quality care to patients.
Endnotes
- J.R. Banegas et al., “Relationship Between Clinic and Ambulatory Blood-Pressure Measurements and Mortality,“ New England Journal of Medicine 378, no. 16 (2018): 1509-1520.
- G. Parati et al., “European Society of Hypertension Guidelines for Blood Pressure Monitoring at Home: A Summary Report of the Second International Consensus Conference on Home Blood Pressure Monitoring,“ Journal of Hypertension 26, no. 8 (2008): 1502-1526.
- Y. Ostchega et al., “Factors Associated With Home Blood Pressure Monitoring Among U.S. Adults: The National Health and Nutrition Examination Survey (NHANES), 2011-2014,“ Hypertension 70, Supplemental 1 (2017).
- G. Parati et al., “European Society of Hypertension Guidelines.“
- M. Reboussin et al., “Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines,“ Journal of the American College of Cardiology 71, no.19 (2018): 2176-2198.
- Y. Ostchega et al., “Factors Associated with Home Blood Pressure Monitoring.“
- B. Dolan, “10 Reasons Why Google Health Failed,“ MobiHealthNews, June 27, 2011. http://www.mobihealthnews.com/11480/10-reasons-why-google-health-failed
- S. Lohr, “Google Is Closing Its Health Records Service After It Fails to Attract Users,“ The New York Times, June 24, 2011. https://www.nytimes.com/2011/06/25/technology/25health.html
- L. Harris, “Google Health Heads to the Hospital,“ MIT Technology Review, May 28, 2008. https://www.technologyreview.com/s/410186/google-health-heads-to-the-hospital/
- E. Schonfeld, “Google Health Creator Adam Botsworth on Why it Failed: ’It’s Not Social’,“ TechCrunch, June 24, 2011. https://techcrunch.com/2011/06/24/google-health-bosworth-social/
- P.C. Tang and T.H. Lee, “Your Doctor’s Office or the Internet? Two Paths to Personal Health Records,“ New England Journal of Medicine 360, no. 13 (2009): 1276-1278.
- D. Chase, “Why Google Health Really Failed — It’s About the Money,“ June 24, 2011. https://techcrunch.com/2011/06/26/why-google-really-failed-money/
- B. Dolan, “10 Reasons Why.“
- D. Chase, “Why Google Health.“
- “Telehealth Services,“ Medicare Learning Network, Centers for Medicare & Medicaid Services (2018).
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network- MLN/MLNProducts/downloads/telehealthsrvcsfctsht.pdf - C. Ayala et al., “Environmental Scan of Telemedicine Networks With Services for Hypertension Management,“ Circulation: Cardiovascular Quality and Outcomes 10 (2017): A221.
- Centers for Medicare & Medicaid Services. “Telehealth Services.“
- “Final Policy, Payment, and Quality Provisions in the Medicare Physician Fee Schedule for Calendar Year 2018,“ Centers for Medicare and Medicaid Services. CMS Press Release Fact Sheet. Nov. 2, 2017. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017-11-02.html
- Ibid.
- Centers for Medicare and Medicaid Services. “Telehealth Services.“
- American Telemedicine Association. State Policy Resource Center. https://www.americantelemed.org/policy-
page/state-policy-resource -center - Centers for Medicare & Medicaid Services. CMS Press Release Fact Sheet.
- American Telemedicine Association. State Policy Resource Center.
- T. Yang et al., “Telehealth Parity Laws. Health Policy Brief,“ Health Affairs, August 15, 2016.
- C. Anderson, “Private Payers Pave New Way for Telemedicine,“ Health care Finance.
https://www.healthcarefinancenews.com/news/private-payers-pay-way-telemedicine?single-page=true - Center for Connected Health Policy. State Telehealth Laws and Medicaid Program. Public Health Institute Center for Connected Health Policy. Fall 2017.
- American Telemedicine Association. State Policy Resource Center.
- Center for Connected Health Policy. State Laws and Reimbursement Policies.
https://www.cchpca.org/telehealth-policy/current-state-laws-and-reimbursement- policies?jurisdiction=62&category=All&topic=All - Aetna. https://news.aetna.com/2017/09/aetna-offers-members-expanded-services-teladoc
- “Welldoc’s BlueStar Now Available for Hypertension and Weight Management,“ Press Release, WellDoc, July 9, 2018. https://www.welldoc.com/news/welldocs-bluestar-now-available-for-hypertension-and-weight- management
- “Omada Health Adds New Programs for Type 2 Diabetes and Hypertension Self-Management,“ Press Release, Omada Health, June 20, 2018. https://omadahealth.com/press/press-release-omada-health-adds-new- programs-fortype-2-diabetes-and-hypertension-self-management
- R. Agarwal et al., “Role of Home Blood Pressure Monitoring in Overcoming Therapeutic Inertia and Improving Hypertension Control: A Systematic Review and Meta-Analysis,“ Hypertension 57, no. 1 (2011): 29-38.
- S.R. Steinhubl, E.D. Muse,and E.J. Topol, “Can Mobile Health Technologies Transform Health Care?“ JAMA 310, no. 22 (2013): 2395-2396.
- H. Landi, “Study: Telemedicine Can Lower Costs for Health Systems by $24 per Patient,“ Health care Informatics. https://www.health care-informatics.com/news-item/telemedicine/study-telemedicine-visits-can- lower-costs-health-systems-24-patient
- https://www.dhs.gov/sites/default/files/publications/digital-strategy/federal-cloud-computing-strategy.pdf (Last accessed March 2018)
- Summary of Policies in the Calendar Year (CY) 2018 Medicare Physician Fee Schedule (MPFS) Final Rule, Telehealth Originating Site Fee Payment Amount and Telehealth Services List. Centers for Medicare & Medicaid Services, January 2018. https://www.cms.gov/Outreach-and-Education/Medicare-Learning- NetworkMLN/MLNMattersArticles/downloads/MM10393.pdf (Last accessed March 2018)
- Final Policy, Payment and Quality Provisions in the Medicare Physician Fee Schedule for CY 2018. Centers for Medicare & Medicaid Services, Nov. 2, 2017. https://www.cms.gov/newsroom/fact-sheets/final-policy- payment-and-quality-provisions-medicare-physician-fee-schedule-calendar-year-2018
- “VA Telehealth Services,“ U.S. Department of Veterans Affairs. https://www.telehealth.va.gov/
- R.Z. Arndt, “House Votes to Ease VA Telemedicine Restrictions,“ Modern Healthcare, Nov. 2, 2017.
http://www.modernhealth care.com/article/20171107/NEWS/171109899 - P.K. Lindenauer et al., “Public Reporting and Pay for Performance in Hospital Quality Improvement,“ New England Journal of Medicine 356, no. 3 (2007): 486-489.
- Mendelson et al., “The Effects of Pay-for-Performance Programs on Health, Health Care Use and Processes of Care: A Systematic Review,“ Annals of Internal Medicine 166, no. 5 (2017): 341-353.
- Medicare Payment Advisory Commission. Public Meeting, Jan. 11, 2018. http://www.medpac.gov/docs/default- source/default-document-library/jan-2018-meeting-transcript.pdf?sfvrsn=0
- “Key Initiatives in Measuring and Reporting Health Care Quality,“ National Committee for Quality Assurance, Agency for Healthcare Research and Quality. http://www.ahrq.gov/professionals/quality-patient- safety/talkingquality/resources/initiatives/ncqa.html
- National Committee for Quality Assurance (NCQA), “Controlling High Blood Pressure.“ http://ncqa.org/report- cards/health-plans/state-of-health-care-quality/2017-table-of-contents/controlling-high-blood-pressure
- NCQA. Agency for Healthcare Research and Quality.
- NCQA. “Controlling High Blood Pressure.“
- NHS England, “Joint Report on International Success Factors for Adoption and Use of Digital Health in the U.S. and NHS England,“ February 2016. https://www.healthit.gov/sites/default/files/adoptionreport_- branded_final4.pdf
- Centers for Medicare & Medicaid Services, “Telemedicine.“
https://www.medicaid.gov/medicaid/benefits/telemed/index.html - NHS England, “Joint Report.“
- Ibid.
- Centers for Medicare & Medicaid Services, “Telemedicine.“
- Office of the National Coordinator for Health Information Technology, “Hospitals Participating in the CMS EHR Incentive Programs“ (2016). https://dashboard.healthit.gov/quickstats/pages/FIG-Hospitals-EHR-Incentive- Programs.php
- NHS England, “Joint Report.“
- Office of the National Coordinator for Health Information Technology, “Hospitals Participating.“
- Centers for Medicare & Medicaid Services, “MACRA.“ https://www.cms.gov/Medicare/Quality-Initiatives- Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and- APMs.html
- https://www.fda.gov/MedicalDevices/DigitalHealth/ucm570617.htm
- K.L. Margolis et al., “Effect of Home Blood Pressure Telemonitoring and Pharmacist Management on Blood
Pressure Control. A Cluster Randomized Trial,“ JAMA 310, no. 1 (2013): 46-56. - M.J. De Jong et al., “Telemedicine for Management of Inflammatory Bowel Disease (myIBDcoach): A Pragmatic, Multicentre, Randomised Controlled Trial,“ Lancet 390, no. 10098: 959-968.
-
-
Driving Innovation
-
Innovations in Cardiovascular Health
-
The Role of Physicians in Driving Innovation
-
The Role of Patient Groups in Driving Innovation
-
Clinical Innovations in Cardiovascular Health
-
What Drives Innovation in CV Health?
-
The Rise of Academic and Contract Research Orgs
-
Federal Regulations as Accelerators
-
Reimbursement Models
-
Consumer Technology
-
Training Cross-Disciplinary Innovators
-
Conclusion